This article looks at the innovative use of sectoral reference architectures, interoperability standards, and transformation toolkits to reduce schedule, budget, and quality risks for IT-enabled transformations in the healthcare and social services sectors. The focus of this article is on an approach used in the United States to respond to a change in government regulations. The case study can be viewed as an example of how to implement a nationwide approach in order to fundamentally change the delivery of healthcare through the use of IT.
1. Introduction
The global economic crisis of the past five years has placed significant fiscal strain on the budgets of healthcare systems globally. On the one hand, the demand for healthcare services continues to grow at a rapid pace due to an ageing population in Western countries and technological improvements. On the other hand, government revenues have fallen, which has forced many countries to cut government spending, including spend on healthcare, which averages around 10% of the GNP in Western countries. As a result, governments and service providers cannot afford to maintain current service levels and meet future demand using current service delivery models. Many governments are implementing large IT-enabled transformations to drive down service delivery costs. These transformation initiatives are often extremely large and risky, as they can affect business processes and IT systems operated by program managers, service providers, and other stakeholders across the healthcare sector of a country. Such transformations typically take much longer and cost much more than planned, and often do not deliver the anticipated level of improvements.
The Organization for Economic Cooperation and Development (OECD), reports that income inequality has increased by more in the first three years of the global economic crisis, to the end of 2010, than it had in the previous 12 years, before factoring in the effects of taxes and transfers on income.[http://www.oecd.org/social/growing-risk-of-inequality-and-poverty-as-crisis-hits-the-poor-hardest-says-oecd.htm] The European Union Employment and Social Situation (December 2012) reports a decline in employment since mid-2011. Nineteen out of the 24 EU member states recorded an employment level below that of four years ago (EU: -2.4%)[http://bookshop.europa.eu/en/eu-employment-and-social-situation-pbKEBH13001/?CatalogCategoryID=WpIKABst.SMAAAEjGJEY4e5L]. Welfare states around the globe have been assisting individuals and families to respond to these income challenges through various human and social service programs and benefits. Responses include employment programs and skills development programs, benefits for housing, food and child support, as well as funding to access healthcare and medical services. However, the gap between the rich and poor is growing in most countries, which has a negative impact on the tax base available to support these programs.
To respond to these challenges, governments are turning to automated service delivery models to deliver healthcare and social services in a more cost-effective and efficient manner. Automated service delivery models are more client-centric, focus on self-service, and provide integrated case management. To achieve these results, synchronized change is required across multiple programs, levels of government, and program stakeholders, including healthcare insurance companies, service providers, and clients. Such a scale of reform has a large impact on program operating models, including processes such as screening, eligibility determination, program enrolment, case management, care delivery, benefits issuance, and the systems that automate them.
2. Healthcare transformation
In response to current fiscal and social challenges, the United States signed into law The Patient Protection and Affordable Care Act (ACA) of 2010, often referred to as “Obamacare,” in March 2010. The ACA required every state to have, by October 2013, a Health Benefit Exchange (HBE) through which individuals or small businesses can compare and purchase private health insurance, and through which individuals can enroll in the publicly funded Medicaid program, or seek subsidies for purchasing private insurance coverage. Through other administrative actions, the US federal government is encouraging other publicly funded human or social services programs to leverage the IT systems built to support an HBE to modernize their own program delivery processes and systems to promote greater reuse and enterprise integration. The overall effort to modernize health and human service systems in a given state can range from $US250 million to $US1 billion for government systems alone. The scale of this transformation is complex and risky as it involves:
- A range of federal, state and local programs for health insurance, employment insurance, healthcare delivery, welfare, disability assistance, child protection and support, and nutrition and housing assistance
- The annual federal government budget for these programs is approaching $1 trillion (many of these programs involve a significant cost-sharing arrangement with state governments)
- A federal reserve fund of $630 billion to implement fundamental healthcare reform over the current decade
- 50 states and their program partners at the local government level
- Approximately 40 national and large regional health insurers and hundreds of state and local insurers
- Tens of thousands of health and human service providers
- Approximately 50 million uninsured or underinsured Americans.
To mitigate the risks associated with planning, designing and implementing this transformation, the federal government has provided healthcare and human service reference architectures and other policy and technical guidance to the states.
3. Achieving IT-enabled Sectoral Transformation
IT-enabled sectoral transformation refers to enhancing and integrating program delivery processes and systems across a sector, with the ultimate goal of more cost-effective service delivery. Healthcare sector transformations impact clients, patients, service providers (both private and non-profit), and government program managers. Information technology supports a range of operating model improvements, including greater self service, integration of service delivery, and case management within a condensed timeframe. Sectoral transformation impacts program operating models for health and human service program delivery and helps to reduce the costs of program administration, therefore achieving the goals set out by healthcare reform initiatives, such as Obamacare.
To be successful in sectoral transformation, all members in the sector must increase the ability of their information systems to interoperate with those of other members. To increase interoperability, the governors or regulators of the sector must establish agreed-upon interoperability standards and reference architectures including business, technical, and semantic standards to ensure that all systems can exchange information in meaningful ways. Past examples of IT-driven cooperation have shown that technical limitations are seldom the blocker, but that disagreement on the cooperation model is. The benefits of sector-based interoperability standards and architectures include:
- alignment of business processes and systems operated by all stakeholders across the sector
- minimizing design, development, and implementation risks
- accelerating delivery times
- increasing economic efficiencies.
Economies of scale are achieved when, for example, integrated screening tools are used to determine client eligibility across multiple programs and benefits are paid out in a streamlined process. It is this level of transformation across the sector, as opposed to individual program changes, that supports significant savings.
There are three critical success factors for achieving sectoral transformation:
- Sector-wide reference architectures
- Interoperability standards
- An analysis, planning, and design toolkit that incorporates these architectures and standards.
In the case of the US healthcare and human services reform, the Department of Health and Human Services published three reference architectures:
- Medicaid Information Technology Architecture (MITA)
- Health Benefits Exchange Reference Architecture (ERA)
- National Human Services Interoperability Architecture (NHSIA).
The US Centers for Medicare and Medicaid Services also published the Medicaid Seven Conditions and Standards[http://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Data-and-Systems/Downloads/EFR-Seven-Conditions-and-Standards.pdf] to standardize and modernize IT systems in the sector. Aside from these reference architectures, there are a number of standards for IT-integration in healthcare (such as HL7, SNOMED CT, ICD-10, CCR/CCD), which provide the foundation for integration.
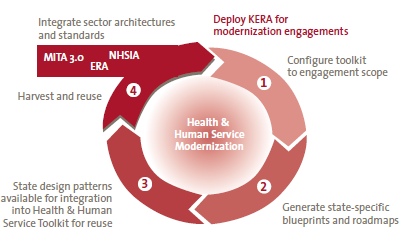
KPMG developed the KPMG Enterprise Reference Architecture toolkit for Health and Human Services (KERA©) to integrate the three reference architectures and seven standards and conditions into a suite of analysis, planning, design, and estimating tools. These tools help members of the sector modernize their information systems to comply with the architectures and standards. This toolkit can be leveraged across jurisdictions and sectors to assist governments, program managers, and service providers in their transformation.
4. Understanding the Steps to Implementing Sectoral Reform: A US Case Study
To comply with the ACA, states must move away from making individual program enhancements and participate in whole-sector reform that includes clients, service providers, government program managers, channel partners, case managers, and sometimes private sector partners, such as healthcare providers, health insurers and employers. Each of the members of the sector have their own business processes and technology in place, which must interoperate with the processes and technology of other members of the sector. States are required to implement this reform under tight deadlines and complex funding agreements between the national and state government, all while maintaining service delivery to citizens. To achieve these goals, government program managers and service providers should consider the following steps or work plan:
- Understand the policy, technical, and funding requirements of the sectoral transformation
- Develop the vision and strategy for their organizations within the sector
- Analyze the gaps for their organizations to meet the transformation requirements
- Generate the design blueprints for business processes and systems
- Estimate the complexity of the transformation solution for their organizations
- Estimate and allocate the costs of the transformation solution
- Develop detailed requirements and designs for transformation solutions
- Implement the blueprints and roadmap for each enterprise within the sector
- Maintain and extend the toolkit.
Each of these steps is explained in greater detail below.
1 Understand the policy, technical and funding requirements
Sectoral reform requires working across multiple levels of government and programs – all with their own complex rules and requirements for funding and service delivery. Mapping out these requirements, how they intersect, and their impact on the sector is a necessary first step to achieving reform. In the case of the US, this has included understanding the grants and funding options available to states from the federal government and mapping out the operational impacts of the new eligibility requirements for health and human services based on income thresholds. In many countries, the transformation in social service delivery is being implemented in parallel with healthcare reform. In the US, this includes developing Health Benefit Exchanges as a self-service front door for program screening and eligibility determination.
2 Develop the Vision and Strategy
Some governments and vendors look at eligibility modernization for health and human service programs as a chance to transfer existing eligibility and benefits issuance processes from obsolescent to more modern IT platforms. While the risks associated with existing legacy platforms are severe, the real return on investment in modernization is in using IT to transform program delivery processes, including shifting from:
- Program centric delivery to client centric delivery
- Agent mediated customer service to increased self service
- Case-based operations to task-based operations.
Developing a unified system modernization vision across the health and human services programs can take several months. However, to meet stringent legislative dates and funding windows outlined for the states required by the ACA in the United States, this visioning process had to be condensed into a few weeks. Executive visioning sessions, typically facilitated by an objective third party and an integrated planning toolkit, helped program managers and insurers to accelerate their decision-making process. The KERA© toolkit helped executives in organizations across the sector to develop new operating models for program and service delivery that leveraged technology to integrate eligibility determination processes across programs. In the United States, these models helped executive leadership to make rapid decisions regarding:
- The scope of a state’s Health Benefits Exchange (HBE) within a broader health and human service modernization discussion
- The place of the HBE within its process vision for health and human service program delivery, including shared government services and outsourcing of non-core activities
- High-level IT requirements for the HBE and for integrated eligibility
- The critical business and IT milestones to implement its healthcare reform and modernization vision.
3 Analyze Gaps to Meet Transformation Requirements
Government program managers and service providers within the sector should perform a gap analysis on their existing IT assets to determine whether there are reusable assets to meet the transformation requirements. A gap analysis tool can be used to upload data and requirements to quickly assess the extent to which current systems can be reused. An effective tool will identify system components that can be reused and opportunities to leverage components of systems in other program areas. The efficiencies to be gained through interoperability can be achieved through streamlined processes as well as by leveraging investments that have already been made in other program areas. As previously noted, these efficiencies come from transformation across the sector as opposed to individual program reform. For example, KPMG has developed a gap analysis tool pre-loaded with the US federal government reference architectures and standards to help states rapidly assess the reusability of their IT assets by comparing existing IT assets against the logical business and technical components in an integrated application architecture.
A gap analysis should also include a software vendor fit-gap analysis capability to assess potential solutions on the market. Architects have used generic sector capability models and software architectures within an industry sector like healthcare to help organizations visualize the logical design of software solutions required by an IT-enabled transformation of health and human services. Sectoral capability and software architecture models are possible to conceive and use because the core operations of organizations within a sector have a high degree of similarity and modern software architectures (e.g., n-tier, service-oriented architectures) are similar across industry sectors.
KPMG has also developed a vendor fit-gap analysis tool to help states assess the suitability of software vendor products against the requirements contained in the three federal reference architectures and the Medicaid Seven Conditions and Standards.
Preloading the gap analysis tools with the appropriate scope of requirements helps ensure that IT staff for government programs and service providers can produce target physical design options for modernization solutions based on reusing existing assets, deploying vendor offerings, or both. The tools help to ensure that these design options are aligned with government guidance and that they can be produced rapidly and consistently. This approach helps to reduce risk and increase cost efficiencies related to design and implementation.
4 Generate the High-Level Blueprints for your Business Processes and Systems
A blueprint that outlines the sectoral reform and impact across all programs allows for rapid decision making and buy-in from multiple stakeholders. Blueprints should be developed for the overall implementation of the transformation to account for key regulatory requirements as they are phased in for the sector. The high-level blueprint can typically take several quarters to execute. US federal government funding constraints required health and human service managers and their program partners to execute this work in a few months. Leveraging sectoral reference architectures allowed states and some of their service providers to develop their program and service blueprints within months rather than quarters.
5 Estimate the Complexity of a Transformation Solution
The results of the gap analysis provide a government program manager or service provider with potential design options for the implementation of an IT solution that will provide automated support for its desired operating model. Modernization projects are now faced with the question of estimating the cost of implementing a given IT solution. To generate a reasonable cost estimate, the project needs to be able to quantify the size of the software solution that will meet the new business requirements.
In response to this challenge, and to help government program managers and service providers comply with the federal regulations; KPMG developed a tool to quantify the scope of a healthcare modernization solution, by applying “function points” as a unit of measure of the functions in the federal reference architectures. Function points are an objective means of measuring the size and complexity of the functions provided by an IT solution. The process for measuring a function point is independent of application development technology, language used for program coding, and the number of code lines. For a given software solution, the higher the function points, the higher the cost to implement and maintain it. Function point analysis is the most widely accepted and generic measure for estimating the size and complexity of an application.
A government program manager or service provider can estimate functional scope of a modernization solution by turning the predefined software functions on and off. Drawing on the conclusions from the executive visioning phase and the configuration of the gap analysis tool, a program manager or service provider will be able to determine the functional complexity of the IT solution required that will meet the business requirements of the newly defined operating model(s).
6 Estimate and Allocate the Costs of a Transformation Solution Roadmap
Modernization project executives must be able to produce reasonably accurate estimates and a high-level roadmap of the IT implementation project to gain necessary funding approvals and establish program operations. Once a government program manager or service provider understands the functional complexity of the IT solution, they must then estimate the design, development, and implementation (DDI) costs as well as operations and maintenance (O&M) costs over the life of the IT modernization solutions.
A “cost modeling” tool should focus on three key variables:
- Functional complexity as measured by the number of function points
- Productivity factor of the implementation strategy, including a reuse strategy (as measured by days of effort per function point)
- Resource mix (as measured by percentage of internal versus external resources and cost of each).
Additional algorithms may be used to estimate a number of costs such as business and IT staff time spent in project management, change management, procurement, user acceptance testing, and benefits realization. The KERA© cost model and roadmap tool is prepopulated with a number of assumptions that help to shape the roadmap and cost estimates for a given state, program or service, and allocate the design, development, implementation, operation and maintenance costs to the appropriate programs within the scope of the sectoral transformation. The tool also comes prepopulated with a configurable work breakdown structure to generate a detailed roadmap of the transformation for program managers or service providers within the sector. By using a prepopulated tool, government program managers and service providers save time and increase the accuracy of their estimates.
7 Develop Detailed Requirements and Designs for the Transformation Solution
Government program managers and service providers must collaborate across agencies and organizations to produce requirements that will meet standards established for the sectoral reform in the visioning stage. This is a shift away from developing unique requirements for each individual program area. Requirements support interoperability across the sector and help to ensure that systems are working together and sharing the right information among the right organizations. Privacy and access policies for the sector enable multiple stakeholders to share client information without compromising their privacy rights.
Requirements are needed by government program managers and service providers for a number of purposes:
- Requirements support the procurement of the correct or “best fit” solution and help to establish a statement of work for a systems integrator
- Requirements will also be used as input into the detailed design and development work of the integrator
- Requirements will support the development and implementation of user-acceptance test plans and test cases.
Leading practices highlight the importance of developing requirements traceability matrices (RTMs) that comply with the regulations and requirements established by each of the program areas involved in the reform. An RTM lists a set of requirements that identifies the automation support required by one or more programs. These matrices accelerate the development of contracts and test plans by providing a comprehensive set of requirements which government program managers can review for applicability. A comprehensive requirements matrix for a given public program or service provider can take several months to develop from scratch, to review with subject matter experts, and to achieve sign off and to align with any federal or national guidance. Prepopulating RTMs with data from sector reference architectures and standards can help a government program manager or service provider reduce the effort to a few weeks.
8 Implement the Blueprints and Roadmap
The high-level blueprints and roadmap should be leveraged to support the implementation of sectoral reform. By establishing common requirements and interoperable standards, the implementation plan should be well understood by all stakeholders. User acceptance and test plans should be worked into the implementation plan to account for process challenges and help ensure ongoing and high-quality customer service. Leveraging a generic implementation plan based on sector architectures and standards can dramatically reduce the time required for a government program manager or service provider to generate a specific implementation plan.
9 Maintain and Extend the Toolkit
Investing in an IT-enabled transformation can provide a government program manager or service provider with tools to carry out reform and respond to changes in the economy on an ongoing basis. KPMG originally developed the KERA© toolkit to integrate the health and human service reference architectures and standards into a usable suite of analysis, planning, and design tools that could be employed by a state government or a service provider within the sector. As KERA© was used to develop state and provider specific blueprints, the KPMG team identified extensions to the toolkit (eg, new design patterns), that could be harvested and incorporated into the toolkit to increase its utility in responding to ongoing changes. These toolkits continue to improve in their functionality and provide government departments with the resources to manage program and service delivery across a sector.

The KERA© Toolkit
5. Conclusion
Under the current economic, financial, and social challenges, governments are being forced to move away from incremental program changes to whole-sector reform. An IT solution that leverages reference architectures can support program managers and service providers to align their business processes and integrate their systems to achieve improved service delivery. Sectoral transformations are big, complex, and risky. The implementation of the ACA in the United States highlights the value of sectoral reference architectures and interoperability standards to minimize the solution design risks of sector stakeholders. Despite the technical difficulties experienced by some of the websites in the recent launch of Obamacare, the states that used the KERA© approach to planning and design of their Health Benefits Exchange solutions were able to accept, process and enroll their citizens in affordable health insurance plans. The KERA© toolkit provided a blueprint to help reduce risk, put in place contingency plans and support the states in their successful implementation.
Embedding these sector reference architectures and interoperability standards in an architectural toolkit can greatly accelerate the development and implementation of the transformation blueprints and roadmaps of each organization in the sector. Implementation of a set of blueprints and roadmaps that are aligned with sector architectures and interoperability standards mitigates the complexity risks associated with sectoral transformations. Accelerated delivery and reduced complexity leads to more cost effective program and service delivery models to improve the fiscal sustainability of essential health and human service programs.